Department №3
Armen Avetisyan
Head of the Pulmonary surgery department №3
Thoracic surgeon, CMS
Adress: Ligovsky Ave., 2-4
Tel.: +7 (812) 775-75-50
The department has 30 beds designed for patients with various forms of pulmonary pathologies (cancer, aspergillosis, etc.). The department is equipped with modern instruments and has qualified medical staff.
Specialists
Grigoriy KudryashovThoracic surgeon, CMS |
Ilya SerezvinThoracic surgeon, CMS |
Alexandr ChausovThoracic surgeon |
Ekaterina DavydenkovaThoracic surgeon, CMS |
Ksenya StashkovaGeneral practitioner |
Diagnostic capabilities
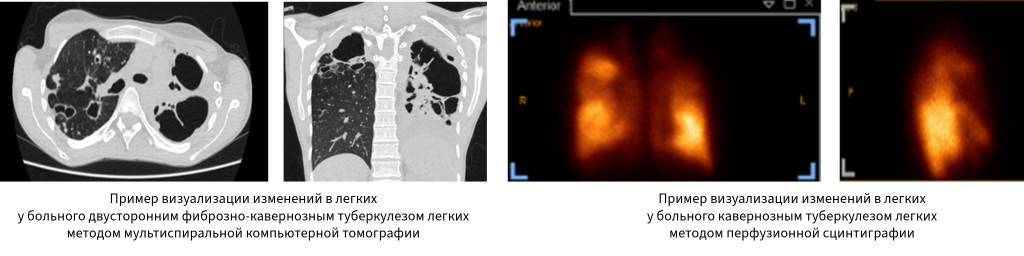
All patients undergo a thorough examination prior to the planned surgery. This includes various laboratory and instrumental diagnostic methods. Laboratory methods include clinical and biochemical blood tests, a coagulogram, a general urine analysis, blood tests for viral hepatitis, HIV infection, and syphilis, and sputum testing for Mycobacterium tuberculosis (PCR for MBT DNA, fluorescence microscopy, and culture on liquid and solid nutrient media). Instrumental diagnostic methods include electrocardiography (ECG), echocardiography (ECHO-CG), chest radiography in two projections, a comprehensive study of external respiratory function, cardiopulmonary stress testing, video tracheobronchoscopy, video esophagogastroduodenoscopy, multispiral computed tomography (MSCT), magnetic resonance imaging, and lung perfusion scintigraphy.
Each patient's examination plan is based on the Department's established standard, which is based on national and international recommendations for examining patients before chest surgery. Based on the patient's comorbidities, if necessary, physicians from related specialties are involved in the examination, and the examination plan is adjusted individually.
Therapeutic activities
The Department performs over 300 operations on the thoracic cavity and chest wall annually. All procedures are performed in modern and well-equipped operating rooms.

The Department's largest share of surgeries involves anatomical lung resections of varying sizes: from segmental resections and lobectomies (removal of a lung lobe) to complex multisegmental combined resections and pneumonectomies for widespread lung disease. The department has developed a system for predicting and preventing the most serious complication after this type of surgery – a bronchopleural fistula – which has enabled us not only to minimize the risk of complications but also to successfully prevent them.
More than two-thirds of all surgeries are performed using mini-invasive techniques. Following a residency at the Shanghai Lung Hospital in China, the Department has widely utilized a single-port video-assisted thoracoscopic approach, which involves a single 3-4 cm incision in the 4th-5th intercostal space along the lateral chest wall. The video-assisted thoracoscopic approach significantly reduces surgical trauma and the risk of postoperative complications, thereby accelerating patient recovery.
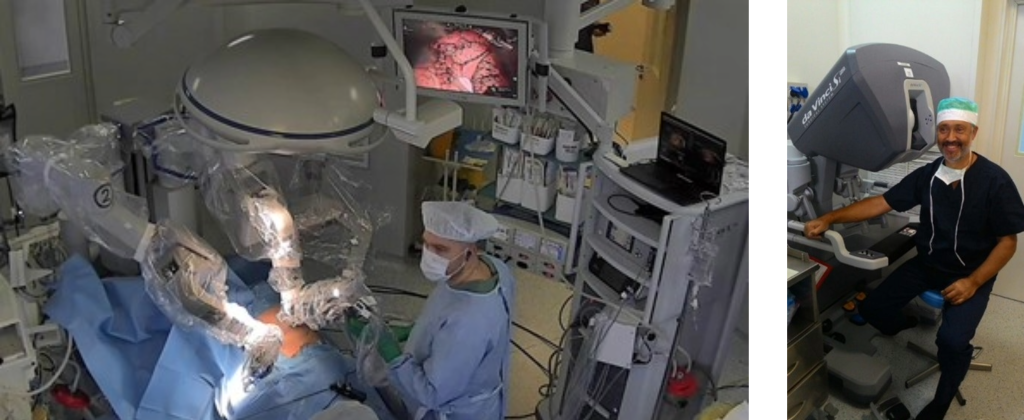
Robot-assisted thoracoscopy is used to perform more complex surgical interventions on the lungs, enabling pinpoint precision when working with important anatomical structures (pulmonary vessels, bronchi). In 2013, Professor Petr Yablonsky and assistant Grigory Kudryashov, performed the world's first lobectomy for pulmonary tuberculosis using a robotic surgical system at Department №3.
In cases where lung resection is contraindicated due to the pathology prevalence, a combination of collapse-surgical interventions is used. The best treatment outcome is achieved with a combination of thoracoplasty followed by valve bronchial blockade and artificial pneumoperitoneum. Importantly, thoracoplasty is performed using an original technique developed in the department. Its advantages, in addition to its high effectiveness in closing lung cavities, include a good cosmetic result: no significant chest wall deformity is observed after surgery.
When surgery on both lungs is necessary, the Department uses a staged approach, which is significantly less invasive and much easier on patients than performing both lungs at once. Each case is treated individually, but is based on the principles of evidence-based medicine.
One of the Department's most important research and practical areas is the development of treatment approaches for patients with various surgical complications following previous surgeries, the most common of which is chronic pleural empyema, with or without a bronchopleural fistula. In tuberculosis, this complication is especially common after lung removal. The Department has developed and implemented the following:
- stage thoracomioplasty procedures that allow the elimination of a main bronchial fistula (usually the right one) and subsequent repair of a chest wall defect (thoracostomy)
- a method for the surgical treatment of recurrent bronchial fistula and pleural empyema after pneumonectomy
Videomediastinoscopic occlusion of the main bronchus (usually the left) has been introduced into practice within the treatment of patients with pleural empyema in combination with bronchopleural fistula, , which is an alternative to the traditionally used traumatic approach with incision of the sternum (sternotomy).
Contact information
You can receive qualified medical care from the Institute's specialists by sending a request to the email address:
|
Galina Dalal |
gl.dalal@spbniif.ru |
 Версия для слабовидящих
Версия для слабовидящих